What Are Ace Inhibitors And How Do They Lower Blood Pressure?
This article aims to provide an objective and impersonal overview of ACE inhibitors, specifically focusing on their role in lowering blood pressure. Hypertension, or high blood pressure, is a prevalent health condition that affects a significant portion of the population.
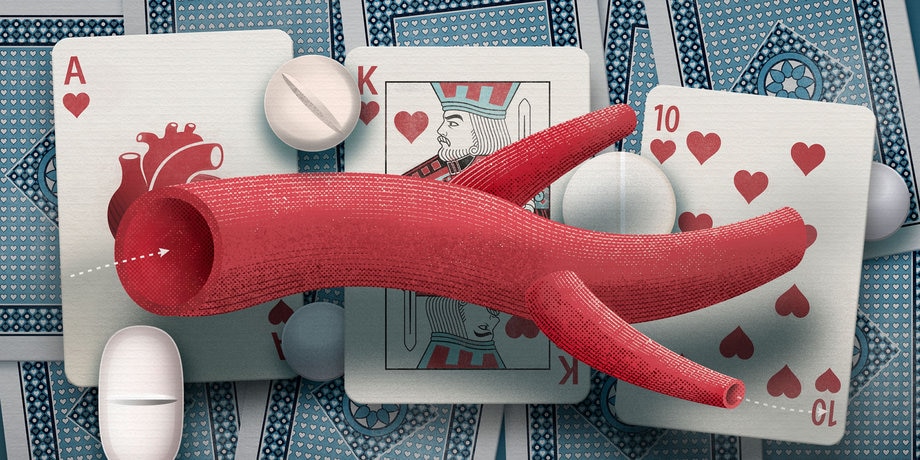
ACE inhibitors are a class of medications commonly prescribed to manage hypertension. To understand the mechanism of action of ACE inhibitors, it is important to first comprehend the physiological processes involved in blood pressure regulation.
This introduction will discuss the role of angiotensin-converting enzyme (ACE) in blood pressure regulation, provide an overview of commonly prescribed ACE inhibitors, and explore their benefits and potential side effects.
Additionally, the article will highlight the importance of complementary lifestyle changes in managing blood pressure and emphasize the significance of consulting with a healthcare provider to develop an individualized treatment plan.
Key Takeaways
- ACE inhibitors are medications that are commonly used to lower blood pressure.
- They work by blocking an enzyme called angiotensin-converting enzyme (ACE), which is involved in the production of a substance called angiotensin II that causes blood vessels to narrow and blood pressure to rise.
- ACE inhibitors are effective in lowering blood pressure and reducing the risk of complications associated with hypertension.
- While ACE inhibitors can have some side effects, they are generally well-tolerated and can be a cost-effective option for managing high blood pressure.
Understanding Blood Pressure and Hypertension
Blood pressure, which measures the force of blood against the walls of the arteries, is primarily regulated by the contraction and relaxation of the heart and the diameter of the blood vessels.
Blood pressure measurement is essential in assessing cardiovascular health, as persistent high blood pressure, known as hypertension, can lead to serious complications such as heart disease and stroke.
Various factors contribute to the development of hypertension, including genetic predisposition, obesity, sedentary lifestyle, and dietary factors. Understanding the causes of hypertension is crucial in developing effective treatment strategies.
Lifestyle modifications, such as regular exercise and a balanced diet, are often recommended as the first line of defense. However, in some cases, medication may be necessary.
One class of medications commonly used to treat hypertension is ACE inhibitors. These medications work by blocking the action of an enzyme called angiotensin-converting enzyme (ACE), which reduces the production of a hormone called angiotensin II.
Angiotensin II is responsible for constricting blood vessels and promoting the release of another hormone called aldosterone, which leads to water and salt retention.
By inhibiting the actions of angiotensin II, ACE inhibitors help to relax and widen blood vessels, reducing blood pressure.
The Role of Angiotensin-Converting Enzyme (ACE) in Blood Pressure Regulation
Angiotensin-converting enzyme plays a crucial role in the regulation of cardiovascular homeostasis, particularly by modulating the activity of the renin-angiotensin-aldosterone system. This system is responsible for maintaining blood pressure within a normal range.
When blood pressure drops, the kidneys release renin, which initiates a cascade of events leading to the production of angiotensin II. Angiotensin II is a potent vasoconstrictor that increases blood pressure by constricting blood vessels. It also stimulates the release of aldosterone, which promotes sodium and water reabsorption, further increasing blood pressure.
ACE inhibitors, as the name suggests, inhibit the activity of angiotensin-converting enzyme, thereby reducing the production of angiotensin II. This leads to vasodilation and decreased sodium and water reabsorption, resulting in lowered blood pressure.
ACE inhibitors are one of the alternative medications used for blood pressure management, along with other classes of drugs such as diuretics and calcium channel blockers.
Commonly Prescribed ACE Inhibitors
Commonly prescribed medications in this class have been shown to effectively modulate the renin-angiotensin-aldosterone system, leading to a reduction in hypertension.
ACE inhibitors are a class of drugs that work by inhibiting the enzyme angiotensin-converting enzyme (ACE), which is responsible for converting angiotensin I into angiotensin II. By blocking this conversion, ACE inhibitors prevent the vasoconstrictive effects of angiotensin II, resulting in vasodilation and decreased peripheral resistance. This ultimately leads to a decrease in blood pressure.
These medications are commonly used in the management of hypertension and are often prescribed as a first-line treatment. They are generally well-tolerated, with common side effects including dry cough and hypotension.
Dosage recommendations for ACE inhibitors can vary depending on the specific medication being prescribed, the patient’s age, and their individual response to the medication. It is essential for healthcare providers to consider these factors when determining the appropriate dosage for patients.
In some cases, alternative medications may be considered if ACE inhibitors are contraindicated or not well-tolerated.
Benefits and Effectiveness of ACE Inhibitors
One notable advantage of ACE inhibitors is their ability to promote vasodilation and decrease peripheral resistance, which can contribute to the management of hypertension. By inhibiting the activity of angiotensin-converting enzyme, ACE inhibitors prevent the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. This results in the relaxation and widening of blood vessels, leading to decreased blood pressure.
In addition to their immediate effects on blood pressure, ACE inhibitors have been shown to have long-term benefits in the treatment of hypertension. They have been associated with a reduction in the risk of cardiovascular events, such as heart attacks and strokes. Furthermore, ACE inhibitors have been shown to improve outcomes in patients with heart failure and diabetic nephropathy.
Despite their effectiveness, the cost of ACE inhibitors can vary depending on the specific medication and insurance coverage, which should be taken into consideration when prescribing these medications. It is important to note that like any medication, ACE inhibitors may have potential side effects and interactions with other medications, and close monitoring is necessary to ensure their safe and effective use.
Potential Side Effects and Precautions
A potential concern associated with the use of ACE inhibitors is the risk of angioedema, a condition characterized by swelling of the face, lips, tongue, or throat, which can be life-threatening in severe cases. This is a rare side effect, occurring in less than 1% of patients. However, it is important for healthcare professionals and patients to be aware of this possibility.
Other potential side effects of ACE inhibitors include a persistent dry cough, dizziness, fatigue, and rash. These side effects are generally mild and resolve on their own.
It is also important to note that ACE inhibitors may interact with other medications, such as diuretics and nonsteroidal anti-inflammatory drugs (NSAIDs), leading to an increased risk of kidney problems or high potassium levels. Therefore, it is important to discuss all current medications with a healthcare provider before starting ACE inhibitor therapy.
Complementary Lifestyle Changes for Blood Pressure Management
Implementing lifestyle changes such as maintaining a healthy weight, engaging in regular physical activity, reducing sodium intake, and adopting a balanced diet rich in fruits, vegetables, and whole grains can play a significant role in managing and potentially reducing high blood pressure.
Dietary modifications, such as reducing the consumption of processed foods and increasing the intake of foods high in potassium, magnesium, and calcium, have been shown to have a positive impact on blood pressure levels.
Additionally, stress reduction techniques, such as mindfulness meditation, yoga, and deep breathing exercises, can help lower blood pressure by promoting relaxation and reducing the body’s response to stress hormones.
These lifestyle changes are often recommended in conjunction with medication, such as ACE inhibitors, as they can enhance the effectiveness of the treatment and provide long-term benefits for blood pressure management.
Consultation with a Healthcare Provider and Individualized Treatment Plan
Consultation with a healthcare provider and the development of an individualized treatment plan are essential steps in effectively managing and improving one’s blood pressure levels, leading to a healthier and more fulfilling life. Individualized treatment options play a crucial role in addressing the unique needs and circumstances of each patient.
Through regular check-ups and consultations, healthcare providers can closely monitor blood pressure levels and make necessary adjustments to the treatment plan. These consultations also provide an opportunity for patients to discuss any concerns or challenges they may be facing in managing their blood pressure. Additionally, healthcare providers can educate patients about lifestyle modifications, such as maintaining a healthy diet and engaging in regular physical activity, which can complement the medical treatment.
By working together with healthcare providers, individuals can receive the necessary guidance and support to effectively manage their blood pressure and improve their overall well-being.
- Customized medication regimens based on individual needs
- Personalized dietary recommendations to reduce sodium intake
- Tailored exercise plans to promote cardiovascular health
- Regular monitoring of blood pressure levels to track progress
- Ongoing education and support to encourage adherence to treatment plan
Frequently Asked Questions
Are ACE inhibitors the only type of medication used to lower blood pressure?
Alternative medications for lowering blood pressure include diuretics, calcium channel blockers, beta blockers, and angiotensin receptor blockers. ACE inhibitors, while effective, may have side effects such as cough and angioedema.
How long does it take for ACE inhibitors to start lowering blood pressure?
ACE inhibitors typically start lowering blood pressure within a few hours of administration. However, the full antihypertensive effect may take several weeks to manifest. Common side effects of ACE inhibitors include cough, dizziness, and elevated potassium levels.
Can ACE inhibitors be used to treat other medical conditions besides high blood pressure?
ACE inhibitors, commonly used to lower blood pressure, can also be used to treat heart failure and diabetic kidney disease. They inhibit the action of the enzyme ACE, leading to vasodilation and reduced fluid retention, thus improving symptoms and slowing the progression of these conditions.
Are there any natural alternatives to ACE inhibitors for lowering blood pressure?
Natural remedies, lifestyle changes, herbal supplements, alternative therapies, dietary modifications, stress reduction techniques, exercise routines, relaxation techniques, meditation practices, and acupuncture treatments may serve as alternatives to ACE inhibitors for lowering blood pressure.
Can ACE inhibitors interact with other medications or supplements?
Interactions with ACE inhibitors and common medications should be carefully monitored, as they may lead to potential side effects. Close attention must be paid to drug interactions, especially with diuretics, nonsteroidal anti-inflammatory drugs, and potassium-sparing diuretics.









