What Is Malignant Hypertension And How Is It Treated?
Malignant hypertension, also known as hypertensive crisis, is a severe medical condition characterized by a rapid and significant increase in blood pressure. This condition requires immediate medical attention due to the potential for organ damage and life-threatening complications. Understanding the pathophysiology, diagnosis, and treatment options for malignant hypertension is essential for healthcare providers to effectively manage this condition.
This article aims to provide an overview of malignant hypertension, its diagnosis, immediate and long-term treatment approaches, potential complications, and the importance of monitoring and follow-up care. Additionally, recognizing and managing hypertensive emergencies, as well as prevention strategies and risk reduction, will be discussed.
By adhering to an academic style of writing that is objective and impersonal, this article aims to present a comprehensive understanding of malignant hypertension and its management.
Key Takeaways
- Malignant hypertension is a severe form of high blood pressure characterized by severely elevated blood pressure levels and can lead to organ damage and life-threatening complications.
- Prompt treatment with medications like nitroprusside, labetalol, or nicardipine, along with lifestyle modifications, is necessary to prevent further deterioration.
- Regular monitoring of blood pressure is crucial, and adherence to prescribed medications is essential for long-term management.
- Hypertensive emergencies require immediate attention, and the goal in managing hypertensive crises is the gradual reduction of blood pressure using intravenous medications like nitroprusside, labetalol, or nicardipine, while closely monitoring vital signs and organ function.
Understanding Malignant Hypertension
Malignant hypertension, also known as hypertensive emergency, is a severe form of high blood pressure that requires immediate medical attention in order to prevent serious complications such as organ damage.
This condition is characterized by a rapid and significant increase in blood pressure, typically reaching levels above 180/120 mmHg.
The exact causes of malignant hypertension are not fully understood, but it is believed that a combination of genetic and environmental factors play a role. Certain risk factors, such as a history of high blood pressure, kidney disease, and certain medications, can increase the likelihood of developing this condition.
Symptoms and signs of malignant hypertension include severe headache, blurred vision, chest pain, shortness of breath, and neurological symptoms like confusion or seizures.
Prompt diagnosis and treatment are crucial to prevent potentially life-threatening complications.
Diagnosing Malignant Hypertension
The diagnosis of severe hypertension involves the assessment of multiple clinical factors and a thorough examination of the patient’s medical history. When it comes to diagnosing malignant hypertension, certain emergency symptoms serve as red flags. These symptoms include severe headaches, chest pain, shortness of breath, vision changes, and neurological deficits.
However, it is important to note that these symptoms are not specific to malignant hypertension and can be seen in other conditions as well. Therefore, a differential diagnosis must be performed to rule out other potential causes of these symptoms. This may involve conducting various tests such as blood pressure measurements, urine analysis, blood tests, electrocardiogram (ECG), echocardiogram, and imaging studies.
Additionally, a comprehensive evaluation of the patient’s medical history and physical examination is crucial in making an accurate diagnosis of malignant hypertension.
Immediate Treatment and Management
This section will discuss the immediate treatment and management of malignant hypertension, focusing on two key points: hospitalization and intensive care, and medications to lower blood pressure.
Hospitalization and intensive care are often necessary for patients with malignant hypertension due to the severity of the condition and the potential complications that can arise.
Medications to lower blood pressure are an essential component of the immediate management of malignant hypertension, aiming to rapidly reduce blood pressure levels and prevent further organ damage.
Hospitalization and Intensive Care
Hospitalization and intensive care are crucial for the treatment of malignant hypertension. When a patient is diagnosed with malignant hypertension, immediate hospitalization is necessary to ensure prompt intervention and prevent further complications. In the hospital setting, patients can be closely monitored and have their blood pressure controlled more effectively.
Intensive care units provide a controlled environment where healthcare professionals can administer medications intravenously, closely monitor vital signs, and promptly address any emergent issues. Treatment in the intensive care unit may include the use of intravenous medications such as nitroprusside or labetalol to rapidly lower blood pressure. Additionally, patients may receive other supportive measures such as fluid management, electrolyte correction, and close monitoring of end-organ damage.
Hospitalization and intensive care play a vital role in managing malignant hypertension and minimizing the risk of life-threatening complications.
Medications to Lower Blood Pressure
Medications that lower blood pressure are an essential component of managing and controlling the condition. They are commonly prescribed to individuals with malignant hypertension to reduce the risk of complications and bring blood pressure levels within a safe range. These medications work by targeting different aspects of blood pressure regulation, such as reducing the volume of blood circulating in the body or relaxing the blood vessels. It is important to note that while medications are effective in controlling blood pressure, they are not the only option available. Natural remedies, such as following a healthy diet low in sodium and rich in fruits and vegetables, regular physical activity, and stress management techniques, can also help lower blood pressure. Non-pharmacological interventions, including weight loss, smoking cessation, and limiting alcohol consumption, are also recommended to complement medication therapy and achieve optimal blood pressure control.
| Medication Class | Example Medications | Mechanism of Action |
|---|---|---|
| Diuretics | Hydrochlorothiazide, Furosemide | Increase urine production, reducing blood volume |
| ACE Inhibitors | Lisinopril, Enalapril | Block the production of a hormone that narrows blood vessels |
| Calcium Channel Blockers | Amlodipine, Nifedipine | Relax and widen blood vessels |
In conclusion, medications play a crucial role in managing malignant hypertension. However, natural remedies and non-pharmacological interventions should also be incorporated to optimize blood pressure control. Consulting with a healthcare professional is essential to determine the most suitable treatment plan for each individual.
Long-Term Treatment and Lifestyle Changes
Long-term treatment and lifestyle changes play a crucial role in managing malignant hypertension. In addition to medications, long-term management involves making certain lifestyle modifications.
First and foremost, it is essential to adopt a heart-healthy diet, such as the Dietary Approaches to Stop Hypertension (DASH) diet, which emphasizes fruits, vegetables, whole grains, lean proteins, and low-fat dairy products while limiting sodium, saturated fats, and cholesterol.
Regular physical activity is also recommended, aiming for at least 150 minutes of moderate-intensity aerobic exercise per week.
Weight management is another important aspect, as losing excess weight can significantly reduce blood pressure.
Additionally, individuals with malignant hypertension should avoid or limit alcohol consumption and quit smoking.
These lifestyle changes, when combined with appropriate medications, can effectively control blood pressure and reduce the risk of complications associated with malignant hypertension.
Potential Complications and Risks
One potential complication of uncontrolled high blood pressure is damage to organs such as the heart, kidneys, and brain. When blood pressure remains consistently high, it forces the heart to work harder to pump blood, leading to an increased risk of heart failure.
Additionally, the high pressure can damage the delicate blood vessels in the kidneys, impairing their ability to filter waste and causing kidney failure.
The brain is also at risk, as uncontrolled hypertension can lead to stroke or transient ischemic attacks (mini-strokes).
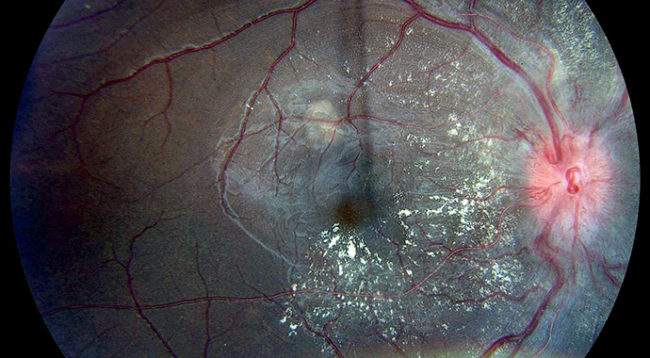
Other potential complications include damage to the eyes, resulting in vision loss, and peripheral artery disease, which can cause pain and difficulty walking.
It is crucial to manage high blood pressure to minimize the risks and complications associated with this condition.
Monitoring and Follow-Up Care
Regular monitoring and follow-up care are essential for individuals with uncontrolled high blood pressure in order to effectively manage their condition and reduce the risk of serious complications. Home monitoring plays a crucial role in this process, as it allows individuals to regularly measure their blood pressure in the comfort of their own homes. By tracking their blood pressure readings, patients can identify any fluctuations and promptly report them to their healthcare provider.
Additionally, lifestyle modifications are an integral part of monitoring and follow-up care. These may include adopting a healthy diet, engaging in regular physical activity, maintaining a healthy weight, limiting alcohol consumption, and quitting smoking. By making these changes, individuals can help control their blood pressure and minimize the likelihood of developing complications associated with malignant hypertension.
Regular monitoring and adherence to lifestyle modifications are vital for long-term management and overall well-being.
Recognizing and Managing Hypertensive Emergencies
Recognizing and managing hypertensive emergencies involves promptly addressing severe and rapid increases in blood pressure to prevent potentially life-threatening complications. Hypertensive emergencies are characterized by severely elevated blood pressure (systolic pressure above 180 mm Hg or diastolic pressure above 120 mm Hg) accompanied by evidence of target organ damage. Prompt recognition is crucial in order to initiate appropriate treatment and prevent further deterioration. The management of hypertensive crises focuses on gradual reduction of blood pressure to prevent complications while avoiding a rapid drop that may lead to organ ischemia. This is typically achieved through the use of intravenous medications such as nitroprusside, labetalol, or nicardipine. In addition to pharmacological treatment, close monitoring of vital signs and organ function is essential to guide therapy and assess response to treatment.
Prevention and Risk Reduction
In the previous subtopic, we discussed recognizing and managing hypertensive emergencies. Now, we will focus on prevention and risk reduction strategies for hypertension.
A key aspect of prevention is making dietary changes. A diet low in sodium and high in fruits, vegetables, and whole grains has been shown to reduce blood pressure.
Additionally, limiting alcohol consumption and avoiding tobacco are important lifestyle modifications that can help prevent hypertension.
Another crucial factor in preventing hypertension is medication adherence. It is essential for individuals diagnosed with hypertension to take their prescribed medications as directed by their healthcare provider. This includes taking medications regularly and at the correct dosage. Adhering to medication regimens can effectively control blood pressure and reduce the risk of developing complications associated with hypertension.
In summary, adopting a healthy diet, avoiding alcohol and tobacco, and adhering to prescribed medications are vital strategies for preventing hypertension and reducing the associated risks.
Frequently Asked Questions
Can malignant hypertension be cured?
Malignant hypertension cannot be cured, but it can be managed effectively through various treatment options. These options may include medications to lower blood pressure, lifestyle modifications, and close monitoring by healthcare professionals to prevent complications.
What are the long-term effects of malignant hypertension if left untreated?
Long-term complications of untreated malignant hypertension can lead to severe organ damage, including damage to the heart, brain, kidneys, and eyes. It is crucial to manage and treat malignant hypertension promptly to prevent these adverse effects.
Are there any alternative treatments or natural remedies for malignant hypertension?
Alternative therapies and lifestyle changes can complement medical treatment for malignant hypertension. Examples include acupuncture, relaxation techniques, exercise, and a healthy diet. However, these should not replace conventional medical care.
Can stress or anxiety trigger an episode of malignant hypertension?
Stress and anxiety can potentially trigger episodes of malignant hypertension. Stress management techniques and lifestyle changes, such as regular exercise, a healthy diet, and adequate sleep, may help reduce the risk of these episodes.
How common is malignant hypertension in children and young adults?
The prevalence of malignant hypertension in children and young adults is low. However, certain risk factors such as kidney disease and genetic predisposition can increase the likelihood. Prevention strategies include managing underlying health conditions and maintaining a healthy lifestyle.