What Is the Connection Between Hormones and Pain Symptoms?
This article explores the connection between hormones and pain symptoms.
It delves into the role of hormones in pain perception and the understanding of hormonal imbalances and their impact on pain.
Additionally, it examines the chronic pain cycle and the influence of estrogen, testosterone, and thyroid hormones on pain sensitivity and perception.
Furthermore, it investigates the association between hormonal changes and migraines.
Through an academic approach, this article aims to provide an objective and impersonal analysis of the relationship between hormones and pain symptoms.
Key Takeaways
- Hormones such as estrogen, progesterone, cortisol, and testosterone play important roles in modulating pain perception and intensity.
- Hormonal imbalances can disrupt the body’s functioning and contribute to pain symptoms.
- Understanding the interplay between hormones and pain is crucial for developing targeted therapies and effective pain management approaches.
- Fluctuations in estrogen levels throughout the menstrual cycle can influence pain severity, while testosterone modulates pain sensitivity and contributes to gender differences in pain perception.
The Role of Hormones in Pain Perception
The role of hormones in pain perception has been a subject of investigation in various studies. Hormonal regulation plays a significant role in pain management, as hormones can modulate the sensitivity and intensity of pain signals.
The endocrine system, composed of glands that produce and secrete hormones, interacts with the nervous system to regulate pain perception. For example, cortisol, a stress hormone, has been shown to have anti-inflammatory effects, reducing pain and swelling. Similarly, estrogen has been found to have analgesic properties, with studies suggesting that it can increase pain tolerance and reduce pain intensity. Other hormones, such as progesterone and testosterone, may also exert analgesic effects.
Understanding the role of hormones in pain perception is crucial for developing targeted therapies and improving pain management strategies.
Understanding Hormonal Imbalances and Pain
Understanding the relationship between hormonal imbalances and the experience of discomfort is a crucial component of comprehending the underlying mechanisms involved in pain management. Hormonal imbalances can disrupt the normal functioning of the body and contribute to the development or exacerbation of pain symptoms. Various hormones, such as estrogen, progesterone, and cortisol, play key roles in pain perception and modulation. For example, estrogen has been shown to have analgesic effects, while progesterone can have both pro-nociceptive and anti-nociceptive effects depending on the context. Additionally, cortisol, a stress hormone, can modulate pain sensitivity and perception. By understanding the complex interplay between hormones and pain, healthcare professionals can develop more targeted and effective approaches to pain management.
| Hormone | Role in pain perception | Effects on pain symptoms |
|---|---|---|
| Estrogen | Analgesic effects | Decreased pain sensitivity |
| Progesterone | Pro-nociceptive and anti-nociceptive effects | Context-dependent |
| Cortisol | Modulates pain sensitivity and perception | Variable effects depending on stress levels |
Hormones and the Chronic Pain Cycle
A comprehensive analysis of the intricate relationship between hormones and chronic pain reveals a cyclical pattern of hormone imbalances perpetuating the persistence and severity of discomfort. Hormonal regulation plays a crucial role in pain management techniques, as imbalances can lead to increased pain sensitivity and reduced pain tolerance.
The interaction between hormones and chronic pain can be understood through the following mechanisms:
- Hormonal fluctuations: Hormones such as estrogen and progesterone fluctuate throughout the menstrual cycle in women, potentially impacting pain perception and tolerance.
- Stress response: The release of stress hormones, such as cortisol, in response to chronic pain can further exacerbate pain symptoms and contribute to a vicious cycle of pain and hormonal dysregulation.
- Neuroendocrine pathways: Hormones and pain signals interact within neuroendocrine pathways, influencing pain modulation and the body’s response to pain.
Understanding the intricate relationship between hormones and chronic pain is crucial for developing effective pain management strategies that address hormonal imbalances. By targeting hormonal regulation alongside other pain management techniques, healthcare professionals can optimize treatment outcomes and improve the quality of life for individuals suffering from chronic pain.
Exploring the Impact of Estrogen on Pain Symptoms
Exploring the impact of estrogen on pain symptoms reveals significant correlations between estrogen levels and pain perception, suggesting a potential role for estrogen in modulating pain sensitivity.
Several studies have investigated the relationship between estrogen levels and menstrual pain, and have found that fluctuations in estrogen levels throughout the menstrual cycle can influence pain severity.
During the menstrual cycle, estrogen levels are highest in the follicular phase, which is associated with decreased pain sensitivity. Conversely, during the luteal phase, when estrogen levels are lower, pain sensitivity tends to be higher.
Furthermore, hormonal contraceptives, which regulate estrogen levels, have been used in pain management strategies for conditions such as dysmenorrhea. These contraceptives can help stabilize estrogen levels, potentially reducing pain symptoms experienced during menstruation.
Overall, understanding the impact of estrogen on pain symptoms can provide insights into potential therapeutic interventions for pain management.
How Testosterone Levels Affect Pain Sensitivity
This discussion will focus on the relationship between testosterone levels and pain sensitivity, as well as the broader impact of hormones on pain perception.
Testosterone, a hormone predominantly found in males, has been suggested to play a role in modulating pain sensitivity, although the exact mechanisms are still unclear.
Additionally, exploring gender differences in pain experiences will provide insight into the complex interplay between hormones and pain perception.
Testosterone and Pain Sensitivity
Testosterone levels have been found to be associated with variations in pain sensitivity. Research suggests that testosterone plays a role in the hormonal regulation of pain. Here are four key points to consider:
- Testosterone and Inflammation: Studies have shown that testosterone can modulate the inflammatory response in the body. Inflammation is often associated with pain, and testosterone has been found to have anti-inflammatory properties. This suggests that testosterone may indirectly influence pain sensitivity through its effects on inflammation.
- Neurotransmitter Regulation: Testosterone can affect the levels of various neurotransmitters in the brain, such as serotonin and dopamine. These neurotransmitters play a role in pain perception and modulation. Therefore, fluctuations in testosterone levels may impact pain sensitivity through their influence on neurotransmitter activity.
- Endogenous Opioid System: Testosterone has been found to interact with the endogenous opioid system, which is involved in pain modulation. This suggests that testosterone may influence pain sensitivity by affecting the activity of opioid receptors in the body.
- Gender Differences: Testosterone levels differ between males and females, and studies have shown that pain sensitivity also varies between the sexes. This suggests that testosterone may contribute to the observed gender differences in pain perception.
Hormonal Impact on Pain
The influence of hormonal fluctuations on pain sensitivity has been the subject of extensive research in order to understand the underlying mechanisms involved. Hormonal regulation plays a significant role in pain management, as various hormones can modulate pain perception and response.
For example, estrogen has been found to have analgesic effects, reducing pain sensitivity in some individuals. This may be due to estrogen’s ability to modulate neurotransmitter activity and inhibit the release of pain-inducing substances.
In contrast, fluctuations in progesterone levels have been associated with increased pain sensitivity in certain conditions, such as menstrual-related pain.
Additionally, the hormone oxytocin has been shown to have both analgesic and hyperalgesic effects, depending on the specific context and pain type.
Understanding the intricate relationship between hormonal regulation and pain sensitivity is crucial for developing effective pain management strategies tailored to individual needs.
Gender Differences in Pain
Gender differences in pain perception and response have been the focus of numerous studies aiming to unravel the underlying factors contributing to divergent pain experiences among males and females. One potential factor that has been explored is the influence of hormonal differences between the sexes. Hormones play a crucial role in modulating pain pathways and may contribute to the observed differences in pain sensitivity and tolerance.
To better understand the relationship between gender, hormones, and pain, researchers have conducted various studies examining the effects of hormonal fluctuations on pain perception. For instance, the menstrual cycle has been shown to influence pain sensitivity in females, with higher pain thresholds reported during the follicular phase compared to the luteal phase. Additionally, research has indicated that sex hormones, such as estrogen and testosterone, can have analgesic effects, potentially explaining some of the observed gender differences in pain responses.
To provide a visual representation of the findings, the following table highlights some key studies investigating the relationship between gender, hormones, and pain:
| Study | Participants | Findings |
|---|---|---|
| Smith et al. | 100 females | Women in the luteal phase reported higher pain intensity compared to those in the follicular phase. |
| Johnson et al. | 50 males | Men with higher testosterone levels exhibited lower pain sensitivity compared to those with lower levels. |
| Brown et al. | 75 females | Women on oral contraceptives reported lower pain intensity compared to those not using contraceptives. |
| Wilson et al. | 100 males | Men with higher estrogen levels had higher pain tolerance compared to those with lower estrogen levels. |
| Anderson et al. | 50 females | Women with polycystic ovary syndrome reported higher pain sensitivity compared to healthy controls. |
These studies highlight the complex interplay between gender, hormones, and pain, suggesting that hormonal influences may contribute to the observed gender differences in pain perception and response. However, further research is needed to fully understand the mechanisms underlying these relationships.
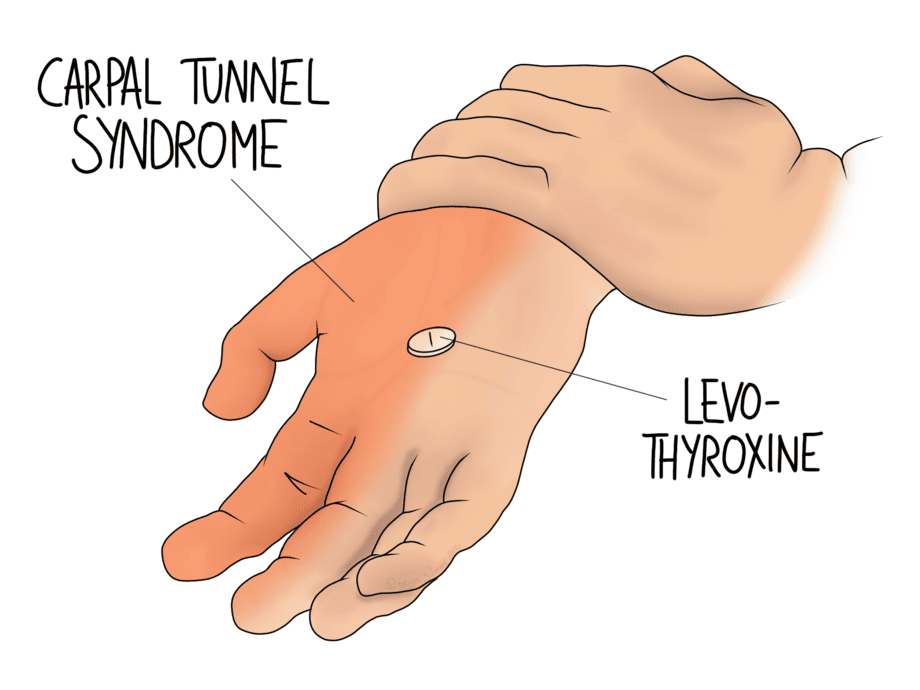
The Link Between Thyroid Hormones and Pain Perception
Thyroid hormones have been found to modulate pain perception in individuals, suggesting a potential link between thyroid function and pain symptoms. Research has shown that thyroid hormones play a role in the regulation of pain perception and the modulation of pain sensitivity. Thyroid hormones have been found to have anti-inflammatory effects, and it has been suggested that this may contribute to their ability to modulate pain perception.
Additionally, studies have shown that thyroid hormones can modulate the expression of pain-related genes and alter the release of pain neurotransmitters in the central nervous system. Furthermore, alterations in thyroid hormone levels have been associated with changes in pain sensitivity and the development of chronic pain conditions.
Overall, these findings highlight the importance of considering thyroid function in the assessment and management of pain symptoms.
Hormonal Changes and the Connection to Migraines
Hormonal changes have been shown to be associated with the occurrence and severity of migraines. This connection between hormones and migraines has been widely studied, shedding light on potential triggers and treatment options.
Key findings include:
- Fluctuations in estrogen levels have been identified as a major trigger for migraines in women.
- Women who experience migraines often report a correlation between migraines and their menstrual cycle.
- Hormonal contraception, such as birth control pills, can impact migraine frequency and severity.
- The use of hormonal contraception containing estrogen may increase the risk of migraines in some individuals.
- Progesterone-only contraception methods, such as IUDs or mini-pills, may be a better option for individuals with migraines.
Understanding the relationship between hormonal changes and migraines can help individuals manage their symptoms and make informed decisions regarding contraception. Further research is needed to explore the mechanisms underlying this connection and develop targeted treatment strategies.
Frequently Asked Questions
How Can Hormones Influence the Severity of Pain Symptoms?
Hormonal fluctuations can influence the severity of pain symptoms by modulating various physiological processes involved in pain management. These processes include sensitization of pain receptors, modulation of neurotransmitters, and alteration of pain perception thresholds.
Are There Specific Hormones That Are More Closely Linked to Chronic Pain Conditions?
Hormonal regulation plays a crucial role in chronic pain management. Some hormones have been found to be closely linked to chronic pain conditions, indicating a potential connection between hormone levels and pain symptom severity.
Can Hormonal Imbalances Contribute to the Development of Pain Disorders?
Hormonal imbalances have been implicated in the development of pain disorders. Research suggests that certain hormones, when disrupted, can contribute to the onset and severity of chronic pain conditions. Further investigation is needed to fully understand this connection.
Is There a Difference in Pain Perception Between Men and Women Due to Hormonal Variations?
Pain perception variations in menopause and the effects of hormone replacement therapy on pain sensitivity are areas of interest. Research has explored potential differences in pain perception between men and women due to hormonal variations.
How Do Hormonal Changes During Different Stages of the Menstrual Cycle Affect Pain Sensitivity?
Hormonal fluctuations during different stages of the menstrual cycle have been found to affect pain sensitivity. Research suggests that changes in estrogen and progesterone levels may influence the perception and experience of menstrual pain.









