What Is The Function Of Antibiotics And How Do They Work?
Bacterial infections pose a significant threat to public health, prompting the need for effective treatment options. Antibiotics have emerged as a crucial tool in the fight against these infections and have revolutionized modern medicine. This article aims to explore the function of antibiotics and elucidate their mechanisms of action.
By adopting an objective and impersonal style, we will delve into the scientific understanding of antibiotics, devoid of personal biases or perspectives. The introduction will provide a concise overview of the topic, setting the stage for a comprehensive analysis of antibiotic function. Furthermore, it will emphasize the importance of this subject matter in the context of public health, as well as the implications of antibiotic resistance.
By adhering to academic writing conventions, this article will provide a valuable resource for those seeking knowledge on the function of antibiotics and how they work.
Key Takeaways
- Antibiotics are essential for treating bacterial infections and preserving their effectiveness.
- Side effects of antibiotics are generally not severe and can be managed, but persistent or severe side effects should be consulted with a healthcare professional.
- Precautions when taking antibiotics include following the prescribed dosage and duration, not sharing or using leftovers for future illnesses, informing healthcare providers about allergies or previous adverse reactions, and finishing the entire course of antibiotics.
- The rise of antibiotic-resistant bacteria necessitates the development of new antibiotics, and exploring alternative approaches such as bacteriophages, immune-based therapies, natural remedies, and probiotics can help reduce potential side effects and resistance.
Understanding Bacterial Infections
Bacterial infections can pose a significant threat to human health, and understanding how these infections occur is crucial in order to effectively combat them.
Bacteria have the ability to rapidly multiply and spread within the body, leading to a wide range of infections.
Bacterial resistance, which refers to the ability of bacteria to withstand the effects of antibiotics, has become a major concern in recent years. This resistance can occur through various mechanisms, such as mutation or acquisition of resistance genes.
Additionally, bacteria have developed various strategies to enhance their virulence, allowing them to evade the immune system and cause severe damage to host tissues.
Understanding the intricate relationship between bacterial resistance and virulence is essential for developing effective strategies to combat bacterial infections and prevent their spread.
Introduction to Antibiotics
Effective treatment of bacterial infections relies on the use of medications that can target and eliminate harmful microorganisms, thereby promoting the restoration of health and preventing the spread of disease. Antibiotics play a crucial role in this process by inhibiting the growth of bacteria or killing them altogether.
The history of antibiotics dates back to the early 20th century when scientists discovered the first antibiotic, penicillin, which revolutionized medicine. Since then, various types of antibiotics have been developed to combat different types of bacterial infections.
These include broad-spectrum antibiotics, which can target a wide range of bacteria, and narrow-spectrum antibiotics, which are specific to certain types of bacteria. Additionally, antibiotics can be classified into different groups based on their chemical structure and mechanism of action.
Understanding the different types of antibiotics is essential for prescribing the most appropriate medication for specific bacterial infections.
Mechanisms of Action
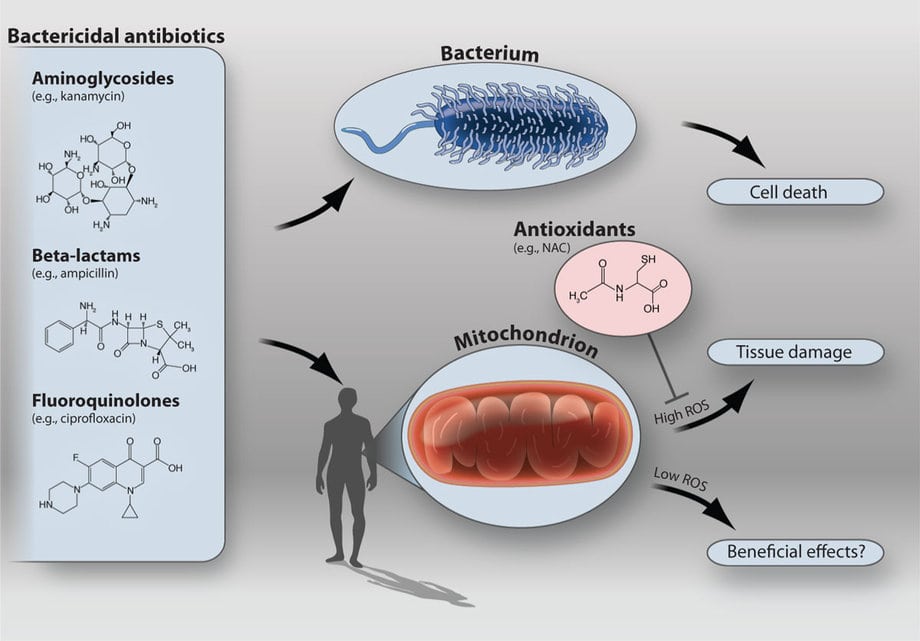
This paragraph will discuss the mechanisms of action of antibiotics, specifically focusing on three key points: inhibition of cell wall synthesis, disruption of protein synthesis, and interference with DNA replication.
Antibiotics can inhibit cell wall synthesis by targeting the enzymes responsible for building the cell wall, resulting in weakened or ruptured cell walls.
Additionally, antibiotics can disrupt protein synthesis by binding to the ribosomes, preventing the synthesis of essential proteins needed for bacterial growth and survival.
Lastly, antibiotics can interfere with DNA replication by targeting enzymes involved in DNA synthesis, leading to DNA damage and inhibition of bacterial replication.
Inhibition of cell wall synthesis
By disrupting the process of cell wall synthesis, antibiotics hinder the growth and reproduction of bacteria, inducing a sense of vulnerability and fragility within the microbial world. Antibiotics target various cellular components involved in cell wall synthesis, leading to inhibition of this crucial process.
The mechanism of action of antibiotics involves interfering with the synthesis of peptidoglycan, the primary component of the bacterial cell wall. This interference can occur at different stages of peptidoglycan synthesis, such as the inhibition of enzymes involved in cross-linking or the prevention of the incorporation of precursors into the growing cell wall.
This disruption weakens the structural integrity of the cell wall, making bacteria susceptible to osmotic lysis and rendering them unable to maintain their shape and survive. Overall, the inhibition of cell wall synthesis is a vital mechanism through which antibiotics exert their bactericidal or bacteriostatic effects.
Disruption of protein synthesis
The interference with protein synthesis is a crucial mechanism employed by antibiotics to disrupt the growth and survival of bacteria, unraveling their ability to produce essential proteins necessary for their function and survival. Antibiotics that disrupt protein synthesis primarily target the translation process, which is the step where the genetic code carried by messenger RNA (mRNA) is used to synthesize proteins.
These antibiotics bind to specific components of the bacterial ribosome, the cellular machinery responsible for protein synthesis. By binding to the ribosome, antibiotics inhibit its function and prevent the accurate reading of the genetic code, leading to the production of faulty or incomplete proteins.
This disruption of the translation process ultimately impacts bacterial growth, as proteins are vital for various cellular processes, including metabolism, cell division, and maintaining cell structure. Consequently, the inhibition of protein synthesis hinders bacterial survival and proliferation.
Interference with DNA replication
In addition to disrupting protein synthesis, antibiotics can also interfere with DNA replication. DNA replication is a fundamental process that ensures the accurate transmission of genetic information from one generation to the next.
Antibiotics that target DNA replication often inhibit the enzymes responsible for DNA synthesis. By blocking these enzymes, antibiotics prevent the replication of bacterial DNA, ultimately leading to cell death.
Moreover, some antibiotics may induce mutagenic effects by causing DNA damage or impairing DNA repair mechanisms. This can result in genetic mutations and alterations in the bacterial genome, further compromising bacterial survival and proliferation.
Understanding the mechanisms by which antibiotics interfere with DNA replication is crucial for the development of new antimicrobial strategies and the effective treatment of bacterial infections.
Spectrum of Activity
Antibiotics have varying degrees of effectiveness against different types of bacteria, which is known as their spectrum of activity. The spectrum of activity of an antibiotic refers to the range of bacteria that it can effectively target and eliminate. Some antibiotics have a narrow spectrum of activity and are only effective against specific types of bacteria. In contrast, broad-spectrum antibiotics are able to target a wide range of bacteria. However, the use of broad-spectrum antibiotics can contribute to the development of drug resistance, as they can also eliminate beneficial bacteria and create an environment for the growth of resistant strains. This emphasizes the importance of using antibiotics judiciously and responsibly to preserve their effectiveness and minimize the emergence of drug-resistant bacteria.
| Antibiotic | Spectrum of Activity | Examples |
|---|---|---|
| Narrow | Effective against a limited range of bacteria | Penicillin G |
| Intermediate | Effective against some Gram-positive and Gram-negative bacteria | Ampicillin |
| Broad | Effective against a wide range of bacteria | Tetracycline |
Antibiotic Resistance
Antibiotic resistance poses a significant challenge in combating bacterial infections, requiring a proactive approach to prevent the emergence and spread of resistant strains.
To address this issue, various strategies have been developed to minimize the development and spread of antibiotic resistance.
- Limiting antibiotic use: Reducing unnecessary and inappropriate use of antibiotics can help prevent the emergence of resistant bacteria.
- Combination therapy: Administering multiple antibiotics simultaneously can hinder the development of resistance by targeting different mechanisms of action.
- Development of new antibiotics: Researchers are constantly working on discovering and developing new antibiotics to combat resistant strains.
- Public education: Educating healthcare professionals and the general public about the appropriate use of antibiotics can help prevent the development and spread of resistance.
Implementing these strategies can aid in preserving the effectiveness of antibiotics and ensuring their long-term usefulness in treating bacterial infections.
Potential Side Effects and Precautions
This paragraph will discuss common side effects of antibiotics as well as precautions and considerations when taking antibiotics.
Common side effects of antibiotics may include gastrointestinal issues such as nausea, diarrhea, and stomach pain. It is important to note that these side effects can vary depending on the specific antibiotic being taken.
When taking antibiotics, precautions should be taken to follow the prescribed dosage and duration of treatment to avoid the development of antibiotic resistance. Additionally, it is crucial to inform healthcare providers of any allergies or sensitivities to antibiotics in order to prevent adverse reactions.
Common side effects of antibiotics
Common side effects of antibiotics can include diarrhea, nausea, and skin rashes. These side effects are considered common because they occur frequently in individuals who take antibiotics.
Diarrhea is one of the most common side effects and can range from mild to severe. Nausea and vomiting may also occur, particularly if the antibiotics are taken on an empty stomach. Additionally, some individuals may develop skin rashes or hives as a result of an allergic reaction to the medication.
It is important to note that while these side effects are common, they are generally not severe and can be managed with appropriate measures. In cases of persistent or severe side effects, it is advisable to consult a healthcare professional for further guidance.
Precautions and considerations when taking antibiotics
When taking antibiotics, it is important to consider the precautions and potential risks associated with their use in order to ensure safe and effective treatment. To manage the potential side effects of antibiotics and prevent antibiotic resistance, the following precautions and considerations should be taken:
- Follow the prescribed dosage and duration of treatment strictly.
- Do not share antibiotics with others or use leftover antibiotics for future illnesses.
- Inform your healthcare provider about any allergies or previous adverse reactions to antibiotics.
- Finish the entire course of antibiotics, even if symptoms improve before completion.
- Avoid consuming alcohol while on certain antibiotics, as it can interfere with their effectiveness.
By adhering to these precautions, side effects and the risk of antibiotic resistance can be minimized, allowing antibiotics to effectively combat bacterial infections.
It is crucial to prioritize responsible antibiotic use to maintain their efficacy for future generations.
The Future of Antibiotics
This paragraph discusses the future of antibiotics, focusing on two key points: the development of new antibiotics and alternative approaches to combat bacterial infections.
In recent years, the rise of antibiotic-resistant bacteria has highlighted the urgent need for the development of new antibiotics. Researchers are exploring various strategies, such as targeting different bacterial pathways and using combination therapies, to overcome antibiotic resistance.
Additionally, alternative approaches, such as the use of bacteriophages and immune-based therapies, are being investigated as potential alternatives to traditional antibiotics.
Developing new antibiotics
In the realm of antibiotic development, exploring novel approaches and strategies has become crucial to combat the rising threat of antibiotic resistance. Drug discovery is at the forefront of these efforts, as researchers search for new antibiotics to effectively combat infectious diseases. Antibiotic resistance, the ability of bacteria to withstand the effects of antibiotics, is a significant challenge in this process.
To overcome this, scientists are exploring alternative sources for potential drug candidates, such as natural products, synthetic compounds, and repurposed drugs. Additionally, advanced technologies, such as high-throughput screening and computer-aided drug design, are being employed to enhance the efficiency of the drug discovery process.
Furthermore, understanding the mechanisms behind antibiotic resistance and the evolution of bacteria is helping researchers develop innovative strategies to overcome this problem. By continuously developing new antibiotics, we can ensure that we stay one step ahead of antibiotic-resistant bacteria and effectively combat infectious diseases.
Alternative approaches to combat bacterial infections
One effective strategy for combating bacterial infections involves exploring alternative approaches that can complement the use of antibiotics. These alternative approaches include the use of natural remedies and probiotics.
- Natural remedies: Many natural substances have antimicrobial properties that can help in fighting bacterial infections. Examples include garlic, honey, and tea tree oil. These natural remedies can be used as topical applications or taken internally to support the body’s immune system.
- Probiotics: Probiotics are beneficial bacteria that can help restore the balance of the gut microbiota and enhance the body’s defense against harmful bacteria. By promoting the growth of good bacteria, probiotics can inhibit the growth of pathogenic bacteria and reduce the risk of infection.
Exploring these alternative approaches not only provides additional options for treating bacterial infections but also helps in reducing the potential side effects associated with antibiotic use.
Frequently Asked Questions
Antibiotics are not effective in treating viral infections. Their efficacy lies in targeting and killing bacteria by disrupting their cell walls or inhibiting their protein synthesis, mechanisms that are absent in viruses.
Are there any natural alternatives to antibiotics?
Herbal remedies and probiotics are potential natural alternatives to antibiotics. They offer the possibility of treating infections without the risk of antibiotic resistance. However, further research is needed to determine their efficacy and safety.
How long does it usually take for antibiotics to start working?
The time it takes for antibiotics to start working can vary depending on several factors, such as the type and severity of the infection, the specific antibiotic used, and individual patient characteristics.
Can antibiotics be used to prevent bacterial infections?
Antibiotics can be used to prevent bacterial infections, but their use for prevention is a concern due to antibiotic resistance. It is important to use antibiotics judiciously to minimize the development of resistance.
What are the differences between broad-spectrum and narrow-spectrum antibiotics?
Broad-spectrum antibiotics target a wide range of bacteria, while narrow-spectrum antibiotics are effective against specific types. Broad-spectrum antibiotics may be more effective initially, but can lead to antibiotic resistance and disrupt the normal microbiota. Narrow-spectrum antibiotics minimize these risks.