What Is The Significance Of Antithrombotic Drugs In Preventing Blood Clots?
Blood clots, also known as thrombosis, pose a significant health risk and can lead to severe complications such as heart attack and stroke. In order to prevent the formation of blood clots, antithrombotic drugs are commonly employed. These drugs, through their anticoagulant and antiplatelet properties, inhibit the clotting cascade and platelet aggregation, respectively.
The significance of antithrombotic drugs lies in their ability to reduce the risk of thrombotic events in individuals who are at high risk due to various factors such as surgery, atrial fibrillation, or previous history of blood clots. This article aims to explore the importance of antithrombotic drugs in preventing blood clots, discussing their benefits, efficacy, and potential risks.
Additionally, the article will delve into the selection and management of antithrombotic therapy, as well as potential future developments in this field. A comprehensive understanding of the significance of antithrombotic drugs is crucial for healthcare professionals and patients alike to make informed decisions regarding thromboprophylaxis.
Key Takeaways
- Antithrombotic drugs are crucial in preventing blood clots and reducing the risk of thrombotic events in high-risk individuals.
- Lifestyle modifications can help prevent blood clots, but antithrombotic drugs are more effective.
- Choosing the right antithrombotic treatment involves evaluating patient-specific characteristics, medical conditions, and risk-benefit profiles.
- Antithrombotic drugs effectively prevent blood clots but increase the risk of bleeding, so balancing risks and benefits is important in therapy.
Understanding Blood Clots and Their Risks
Understanding the risks associated with blood clots is crucial in order to effectively prevent their occurrence.
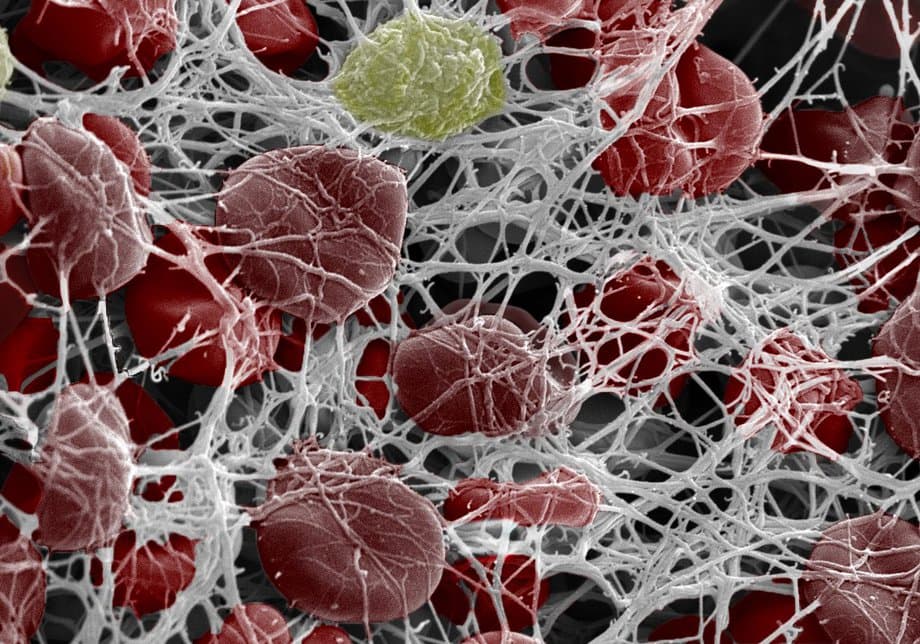
Blood clots, or thrombi, are clumps of blood that form when the body’s natural clotting process becomes overactive. They can occur in both the arteries and veins and can lead to serious complications, such as heart attack, stroke, or pulmonary embolism.
Certain factors increase the risk of developing blood clots, including age, obesity, smoking, and a sedentary lifestyle.
Prevention strategies for blood clots involve lifestyle modifications, such as regular exercise, maintaining a healthy weight, and avoiding smoking.
In addition, antithrombotic drugs play a significant role in preventing blood clots by inhibiting the clotting process or dissolving existing clots. These drugs include anticoagulants, antiplatelet agents, and thrombolytics, which are prescribed based on the individual’s risk factors and medical history.
By understanding the risks and implementing prevention strategies, along with the use of antithrombotic drugs, the occurrence of blood clots can be effectively reduced.
Introduction to Antithrombotic Drugs
This paragraph will discuss the key points related to antithrombotic drugs, including how they work, the types of medications available, and the common side effects and precautions associated with their use.
Antithrombotic drugs are designed to prevent the formation of blood clots by inhibiting the clotting process.
There are different types of antithrombotic medications available, including antiplatelet drugs, anticoagulants, and thrombolytic agents.
While these medications can be effective in preventing blood clots, they can also have side effects and require careful monitoring and precautions to ensure their safe and effective use.
How Antithrombotic Drugs Work
Antithrombotic drugs play a crucial role in preventing blood clots by inhibiting platelet aggregation and reducing the risk of thrombus formation. These drugs act through various mechanisms to interfere with the clotting process. One important mechanism is the inhibition of platelet activation and aggregation, which prevents the formation of a platelet plug at the site of injury. Additionally, antithrombotic drugs can interfere with the coagulation cascade by inhibiting specific clotting factors. This helps to prevent the formation of a stable blood clot.
Another important aspect to consider when using antithrombotic drugs is potential drug interactions. Some antithrombotic drugs may interact with other medications, leading to adverse effects or reduced efficacy. Healthcare professionals must be aware of these interactions and carefully monitor patients to ensure the safe and effective use of antithrombotic therapy. By understanding the antithrombotic mechanism of action and potential drug interactions, healthcare providers can optimize treatment strategies and minimize the risk of blood clot formation.
| Antithrombotic Mechanism | Drug Interactions |
|---|---|
| Inhibition of platelet activation and aggregation | Interactions with other medications |
| Interference with the coagulation cascade | Adverse effects or reduced efficacy |
| Prevention of stable blood clot formation | Need for careful monitoring and optimization of therapy |
Types of Antithrombotic Medications
One important aspect to consider when managing patients at risk of thrombus formation is the classification of antithrombotic medications.
There are several types of antithrombotic medications available, each with its own mechanism of action and target in the clotting cascade. The main antithrombotic drug options include antiplatelet agents, anticoagulants, and thrombolytics.
Antiplatelet agents, such as aspirin and clopidogrel, work by inhibiting platelet aggregation and preventing the formation of blood clots.
Anticoagulants, such as heparin and warfarin, interfere with the clotting cascade and inhibit the synthesis of clotting factors, thus preventing the formation of new clots and the extension of existing clots.
Thrombolytics, such as alteplase, directly dissolve blood clots by activating plasminogen and promoting fibrinolysis.
The choice of antithrombotic medication depends on various factors, including the underlying condition, the severity of the clotting risk, and individual patient characteristics.
It is crucial for healthcare providers to have a thorough understanding of the different types of antithrombotic medications to ensure optimal management of patients at risk of blood clots.
Common Side Effects and Precautions
Common side effects and precautions associated with the use of antithrombotic medications should be taken into consideration in order to ensure safe and effective management of patients at risk of thrombus formation.
Antithrombotic drugs, while crucial in preventing blood clots, can also have certain adverse effects. It is important for healthcare providers to be aware of these potential side effects and take appropriate precautions.
Common side effects may include bleeding, bruising, and gastrointestinal disturbances. These medications can also interact with other drugs, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and anticoagulants, leading to increased risk of bleeding.
Patients should be advised to report any unusual bleeding or bruising, and healthcare providers should monitor their blood clotting parameters regularly. Additionally, patients with a history of gastric ulcers or other bleeding disorders require close monitoring when using antithrombotic medications to minimize the risk of complications.
Preventing Blood Clots in High-Risk Individuals
Preventing blood clots in individuals at high risk is a crucial aspect of managing their overall health and reducing the chances of potentially life-threatening complications. High-risk individuals include pregnant women and those undergoing surgical procedures.
Pregnancy is associated with an increased risk of blood clots due to hormonal changes and mechanical compression of blood vessels by the growing fetus. Antithrombotic drugs are commonly used to prevent blood clots in pregnant women, particularly those with a history of previous clotting events or other risk factors. These drugs help to inhibit the formation of blood clots and prevent their progression.
Similarly, individuals undergoing surgical procedures are also at an increased risk of developing blood clots due to immobility and surgical trauma. Antithrombotic drugs, such as low molecular weight heparin, are often prescribed to prevent clot formation during and after surgery, reducing the risk of complications such as deep vein thrombosis and pulmonary embolism.
Overall, the use of antithrombotic drugs in high-risk individuals plays a vital role in preventing blood clots and ensuring their well-being.
Benefits and Efficacy of Antithrombotic Drugs
The benefits and efficacy of antithrombotic medications have been extensively studied and documented, making them a valuable tool in managing the health of high-risk individuals. These drugs play a crucial role in preventing blood clots and reducing the risk of life-threatening conditions such as stroke and deep vein thrombosis.
When it comes to long-term use, antithrombotic drugs have shown significant benefits. They help maintain proper blood flow by inhibiting the formation of blood clots, thus preventing potentially fatal complications. Additionally, these medications have been found to be more effective than other preventive measures, such as lifestyle modifications or intermittent pneumatic compression devices.
To better understand the benefits and efficacy of antithrombotic drugs, a comparison can be made using the following table:
| Antithrombotic Medications | Benefits |
|---|---|
| Reduces risk of stroke | Yes |
| Prevents deep vein thrombosis | Yes |
| More effective than lifestyle modifications | Yes |
| Compared to intermittent pneumatic compression devices | More effective |
In summary, the benefits of long-term use of antithrombotic drugs in preventing blood clots are well-documented. These medications outperform other preventive measures and significantly reduce the risk of life-threatening complications.
Choosing the Right Antithrombotic Treatment
When considering the benefits and efficacy of antithrombotic drugs in preventing blood clots, it is essential to also focus on the process of choosing the right antithrombotic treatment. With the wide range of available medications, selecting appropriate drugs for individual patients becomes crucial in achieving optimal outcomes.
The selection process involves a comprehensive evaluation of various factors, including patient-specific characteristics, underlying medical conditions, and the risk-benefit profile of each drug. Additionally, personalized treatment options have gained significant attention in recent years. This approach aims to tailor antithrombotic therapy according to an individual’s unique characteristics, such as genetic factors, comorbidities, and lifestyle considerations.
By implementing a personalized approach, healthcare professionals can optimize treatment outcomes while minimizing the risk of adverse events. Therefore, the process of choosing the right antithrombotic treatment plays a pivotal role in the effective prevention of blood clots.
Managing Antithrombotic Therapy
Managing antithrombotic therapy requires careful consideration of individual patient characteristics and risk-benefit profiles to optimize treatment outcomes and minimize the potential for adverse events.
This involves a thorough assessment of various factors, such as the patient’s age, medical history, concomitant medications, and lifestyle habits, which can influence the choice and dosing of antithrombotic drugs.
To manage therapy complications effectively, healthcare providers must monitor patients closely for potential adverse effects, such as bleeding or drug interactions. Regular laboratory tests, such as complete blood counts and coagulation panels, can help assess the patient’s response to treatment and guide dose adjustments.
Additionally, personalized treatment options, such as genetic testing for specific genetic variations affecting drug metabolism or response, can aid in tailoring the therapy to individual patients.
Overall, by considering individual patient characteristics and risk-benefit profiles, healthcare professionals can optimize antithrombotic therapy, reduce the risk of complications, and improve patient outcomes.
Potential Risks and Side Effects
This paragraph discusses potential risks and side effects associated with antithrombotic therapy. One of the main concerns is bleeding complications, as antithrombotic drugs can interfere with the blood’s ability to clot and increase the risk of bleeding.
Allergic reactions to these drugs are also possible, and can range from mild skin rashes to severe anaphylaxis.
It is important for healthcare professionals to carefully balance the risks and benefits of antithrombotic therapy, taking into account the patient’s individual characteristics and medical history.
Bleeding Complications
Bleeding complications can arise as a result of the administration of antithrombotic drugs. These drugs, while effective in preventing blood clots, can increase the risk of bleeding in patients. The severity of bleeding complications can vary, ranging from minor bruising to life-threatening hemorrhage. Management strategies are crucial in minimizing the risk and handling these complications effectively.
Here are five potential outcomes of bleeding complications that may evoke an emotional response:
- Excessive bleeding leading to prolonged hospitalization and medical interventions
- Impaired physical and emotional well-being of the patient
- Increased anxiety and stress for the patient and their family members
- Financial burden due to medical expenses and loss of productivity
- Potential long-term consequences, such as anemia or organ damage
It is essential for healthcare professionals to carefully monitor patients receiving antithrombotic drugs and promptly address any bleeding complications to ensure patient safety and well-being.
Allergic Reactions
Allergic reactions are a potential complication of antithrombotic drugs, which are commonly used to prevent blood clots. These medications can trigger hypersensitivity reactions in some individuals, leading to a range of symptoms from mild skin rashes to severe anaphylaxis.
The incidence of allergic reactions varies depending on the specific antithrombotic drug and individual patient factors. Identifying and managing these reactions is crucial to ensure patient safety and optimize treatment outcomes.
In cases of mild allergic reactions, discontinuing the medication and providing supportive care may be sufficient. However, in severe cases, alternative treatment options may need to be considered to prevent further complications.
It is essential for healthcare professionals to be vigilant and promptly address any allergic reactions associated with antithrombotic drugs to ensure patient well-being and to provide effective treatment.
Balancing Risks and Benefits
One important consideration in the use of antithrombotic medications is the need to carefully balance their potential risks and benefits.
Antithrombotic drugs, such as aspirin, warfarin, and heparin, are widely used in preventing blood clots and reducing the risk of stroke and heart attack. However, like any medication, they come with potential risks.
The main concern with antithrombotic drugs is the increased risk of bleeding. While these drugs effectively prevent blood clots, they can also inhibit the clotting process, leading to excessive bleeding.
Physicians must weigh the potential benefits of preventing blood clots against the risks of bleeding when deciding whether to prescribe antithrombotic drugs. Factors such as the patient’s underlying conditions, age, and overall health status play a crucial role in determining the appropriate use and dosage of these medications.
Careful consideration and individualized treatment plans are necessary to achieve the optimal balance between risks and benefits in antithrombotic therapy.
Future Developments in Antithrombotic Therapy
Advancements in drug formulations are an important area of future development in antithrombotic therapy. Researchers are constantly working to improve the effectiveness and safety of existing antithrombotic drugs by developing new formulations with enhanced properties.
Additionally, there is a growing interest in exploring potential alternatives to traditional antithrombotic drugs, such as novel agents that target specific components of the clotting cascade or alternative therapeutic approaches.
Furthermore, ongoing research and innovation in the field of antithrombotic therapy are essential for identifying new targets, understanding mechanisms of action, and developing novel treatment strategies to improve patient outcomes.
Advancements in Drug Formulations
A notable development in the field of antithrombotic drugs involves the formulation of novel delivery systems, allowing for targeted drug delivery and improved efficacy in preventing blood clots. One significant advancement is the use of nanotechnology in drug delivery. Nanoparticles, with their small size and high surface area, offer several advantages in terms of drug delivery. They can be engineered to encapsulate antithrombotic drugs and deliver them directly to the site of clot formation, thereby increasing drug concentration at the target site and minimizing systemic side effects. Additionally, nanotechnology allows for the incorporation of stimuli-responsive systems, enabling controlled drug release in response to specific triggers, such as changes in pH or temperature. These advancements in drug formulation hold great promise in enhancing the effectiveness and safety profile of antithrombotic therapy.
| Advancements in Drug Formulations |
|---|
| – Nanoparticle-based drug delivery |
| – Targeted drug delivery |
| – Stimuli-responsive drug release |
| – Enhanced efficacy and safety |
Potential Alternatives to Traditional Antithrombotic Drugs
Potential alternatives to traditional antithrombotic drugs include the exploration of novel therapeutic modalities that can effectively target clot formation while minimizing systemic side effects. In recent years, there has been increasing interest in alternative therapies and natural remedies for preventing blood clots. These options seek to harness the potential of natural compounds and mechanisms to inhibit clot formation without the need for synthetic drugs.
Some potential alternatives to traditional antithrombotic drugs include:
- Herbal remedies: Certain herbs, such as garlic, ginger, and turmeric, have been suggested to have antithrombotic properties. These natural compounds may possess antiplatelet and anticoagulant effects, which can help prevent blood clot formation.
- Dietary interventions: Consuming a diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids has been associated with a reduced risk of blood clots. These dietary components may have anti-inflammatory and anticoagulant effects, potentially offering a natural approach to preventing clot formation.
Exploring these alternative therapies and natural remedies may provide new avenues for preventing blood clots while minimizing the potential side effects associated with traditional antithrombotic drugs. Further research is needed to fully understand the efficacy and safety of these approaches.
Research and Innovation in the Field
Research and innovation in this field are driving the development of novel therapeutic modalities and exploring new approaches to inhibit clot formation. Recent research advancements have led to the discovery of potential alternative treatment options for preventing blood clots. One such advancement is the development of targeted anticoagulant drugs that specifically inhibit the activity of certain clotting factors, reducing the risk of excessive bleeding that is often associated with traditional antithrombotic drugs. Additionally, researchers are investigating the use of nanotechnology to deliver antithrombotic agents directly to the site of clot formation, enhancing their efficacy and minimizing systemic side effects. Other innovative approaches include the use of gene therapy to modulate the expression of clotting factors and the development of synthetic biomaterials that can mimic the natural antithrombotic properties of the body. These research efforts hold promise for the development of safer and more effective treatment options for preventing blood clots.
| Research Advancements | New Treatment Options |
|---|---|
| Targeted anticoagulant drugs | Nanotechnology for targeted drug delivery |
| Gene therapy | Synthetic biomaterials |
Frequently Asked Questions
What are the common symptoms of a blood clot?
Common symptoms of a blood clot include swelling, warmth, redness, and pain in the affected area. Diagnosis methods may involve imaging tests, such as ultrasound or venography, along with blood tests to measure clotting factors.
Can antithrombotic drugs be used to treat existing blood clots?
Antithrombotic drugs can be used to treat existing blood clots by preventing further clot formation and promoting clot dissolution. The effectiveness of antithrombotic drugs varies depending on the type of drug used and the specific characteristics of the clot.
Are there any alternative treatments to antithrombotic drugs for preventing blood clots?
Non-drug alternatives and lifestyle changes can be used to prevent blood clots. These can include maintaining a healthy weight, regular exercise, avoiding prolonged periods of immobility, and wearing compression stockings.
What factors should be considered when choosing the right antithrombotic treatment for an individual?
Factors to consider when choosing the appropriate antithrombotic treatment for an individual include their medical history, risk factors for clotting, potential drug interactions, comorbidities, and patient preferences. These considerations ensure optimal treatment efficacy and safety.
Are there any potential long-term effects of taking antithrombotic drugs?
Potential risks and side effects of antithrombotic drugs include bleeding, bruising, gastrointestinal issues, and increased risk of hemorrhage. However, their long-term effects are still being studied, and further research is needed to fully understand their impact.