Why Hypertension Is A Risk Factor For Cardiovascular Disease?

Hypertension, or high blood pressure, is a prevalent medical condition that affects a significant proportion of the global population. It is well-established that hypertension is a major risk factor for the development of cardiovascular disease, which includes conditions such as heart attack, stroke, and heart failure.
The association between hypertension and cardiovascular disease has been extensively studied, and research has identified several mechanisms through which hypertension can contribute to cardiovascular damage. These mechanisms encompass both structural and functional changes in the blood vessels, as well as alterations in the heart’s pumping ability.
Furthermore, hypertension can lead to various complications, such as kidney disease and peripheral artery disease, which further increase the risk of cardiovascular events. Given the substantial implications of hypertension on cardiovascular health, effective management strategies are crucial to mitigate these risks. Regular blood pressure monitoring and lifestyle modifications are fundamental in preventing and controlling hypertension, thereby reducing the likelihood of cardiovascular disease development.
Key Takeaways
- Hypertension is a known risk factor for cardiovascular disease.
- Regular blood pressure monitoring allows for early detection and intervention, leading to better outcomes.
- Lifestyle modifications, such as maintaining a well-balanced diet and engaging in regular physical activity, can help manage hypertension and reduce the risk of cardiovascular complications.
- Implementing prevention strategies, including managing stress, limiting alcohol consumption, and quitting smoking, can significantly reduce the risk of hypertension and cardiovascular disease.
Understanding Hypertension
Hypertension, characterized by persistently elevated blood pressure levels, is a significant risk factor for the development of cardiovascular disease. Understanding the causes and treatment of hypertension is crucial in managing this condition effectively.
There are two main types of hypertension: primary (essential) and secondary hypertension. Primary hypertension, which accounts for the majority of cases, has no identifiable cause, while secondary hypertension is often a result of an underlying medical condition.
Risk factors for hypertension include age, family history, obesity, sedentary lifestyle, and certain medical conditions.
Lifestyle modifications, such as regular physical activity, a healthy diet, and weight management, are essential in managing hypertension. Additionally, pharmacological interventions, including antihypertensive medications, may be prescribed to control blood pressure levels.
Understanding the causes and treatment of hypertension is paramount in reducing the risk of cardiovascular disease associated with this condition.
The Link Between Hypertension and Cardiovascular Disease
The relationship between elevated blood pressure and the occurrence of heart-related ailments is well-documented in scientific literature. Hypertension, or high blood pressure, is a significant risk factor for cardiovascular disease.
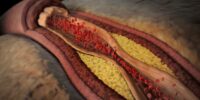
The link between hypertension and cardiovascular disease lies in the strain that high blood pressure places on the arteries. Over time, this strain can lead to the development of atherosclerosis, a condition characterized by the buildup of fatty deposits in the arterial walls. These deposits can narrow the arteries, compromising blood flow to the heart muscle.
Additionally, hypertension can also lead to the weakening and enlargement of the heart, a condition known as left ventricular hypertrophy. This can further increase the risk of heart failure and other cardiovascular complications.
Therefore, managing and treating hypertension is crucial in reducing the risk of cardiovascular disease.
Mechanisms of Hypertension-Related Cardiovascular Damage
One of the key mechanisms behind the damage caused by elevated blood pressure on the cardiovascular system involves the development of atherosclerosis, a condition characterized by the accumulation of fatty deposits in the arterial walls.
Hypertension-related kidney damage is another mechanism that contributes to cardiovascular disease. The kidneys play a crucial role in regulating blood pressure, and when hypertension occurs, it can lead to structural and functional changes in the kidneys, such as narrowing of blood vessels and impaired filtration of waste products. These changes can further exacerbate hypertension and contribute to the development of cardiovascular disease.
Additionally, inflammation plays a significant role in hypertension-related cardiovascular damage. Chronic inflammation can lead to endothelial dysfunction, oxidative stress, and the release of inflammatory mediators, all of which contribute to the progression of atherosclerosis and cardiovascular damage.
Understanding these mechanisms is essential for developing effective strategies to prevent and manage hypertension-related cardiovascular disease.
Complications of Hypertension
This discussion will focus on the complications of hypertension. Specifically, it will cover atherosclerosis and plaque buildup, heart failure, and arrhythmias.
Atherosclerosis refers to the buildup of plaque in the arteries, leading to narrowed blood vessels and reduced blood flow.
Heart failure occurs when the heart is unable to pump blood efficiently, often due to the increased workload caused by hypertension.
Arrhythmias are abnormal heart rhythms that can be caused by the structural changes and electrical disturbances associated with hypertension.
Atherosclerosis and plaque buildup
Atherosclerosis, characterized by the accumulation of plaque in the arterial walls, is a significant contributor to the association between hypertension and cardiovascular disease. Hypertension creates an environment that promotes the development and progression of atherosclerosis. The elevated blood pressure damages the endothelial lining of the arteries, allowing lipids and inflammatory cells to infiltrate the vessel wall. This leads to the formation of atherosclerotic plaques, composed of cholesterol, immune cells, and connective tissue. The plaque buildup narrows the arteries, restricting blood flow to vital organs and tissues. Moreover, the plaques can rupture, triggering the formation of blood clots that can completely block blood flow, leading to heart attacks or strokes. Atherosclerosis prevention strategies, such as blood pressure control and lifestyle modifications, are crucial in reducing the risk of plaque formation and rupture.
| Atherosclerosis Prevention | Plaque Rupture |
|---|---|
| Blood pressure control | Vulnerable plaques |
| Lifestyle modifications | Thrombosis |
| Healthy diet | Inflammation |
| Regular exercise | Endothelial dysfunction |
Heart failure and arrhythmias
Heart failure and arrhythmias are common complications that can arise as a result of the association between hypertension and the pathophysiological processes involved in plaque formation and rupture.
Hypertension leads to an increased workload on the heart, causing it to pump harder to meet the body’s demands. Over time, this can lead to the development of heart failure, a condition characterized by the heart’s inability to pump blood effectively.
Additionally, hypertension can disrupt the electrical signals in the heart, resulting in arrhythmias, which are abnormal heart rhythms.
To manage heart failure, lifestyle modifications such as a low-sodium diet, regular exercise, and medication therapy are recommended. Medications commonly used include diuretics, ACE inhibitors, and beta-blockers.
For arrhythmia treatment, options include medications, implantable devices like pacemakers or defibrillators, and procedures such as catheter ablation.
It is important for individuals with hypertension to monitor their blood pressure regularly and work closely with healthcare professionals to prevent or manage these complications effectively.
Managing Hypertension to Reduce Cardiovascular Risk
One effective strategy for reducing cardiovascular risk associated with hypertension is through the management of blood pressure levels. This can be achieved through a combination of medication and lifestyle changes. Medications such as diuretics, beta blockers, and ACE inhibitors are commonly used to lower blood pressure in individuals with hypertension. Additionally, lifestyle modifications such as adopting a healthy diet low in sodium and saturated fats, engaging in regular physical activity, maintaining a healthy weight, and limiting alcohol consumption can also help to manage hypertension.
To provide a comprehensive overview of managing hypertension to reduce cardiovascular risk, the following table summarizes the different strategies and their effectiveness:
| Strategy | Effectiveness |
|---|---|
| Medication | High |
| Lifestyle changes | Moderate |
| Combination therapy | High |
| Self-monitoring | Moderate |
Overall, a multifaceted approach that combines medication and lifestyle changes is recommended for effectively managing hypertension and reducing the associated cardiovascular risk.
The Importance of Regular Blood Pressure Monitoring
Regular blood pressure monitoring is essential in order to effectively manage and prevent complications associated with elevated blood pressure levels. Hypertension, or high blood pressure, is a known risk factor for cardiovascular disease, and regular monitoring allows for early detection and intervention.
By regularly checking blood pressure levels, healthcare professionals can assess the effectiveness of treatment plans and make necessary adjustments to optimize control. This monitoring also helps individuals understand the impact of lifestyle modifications and medication adherence on their blood pressure.
Moreover, regular blood pressure monitoring provides an opportunity for healthcare professionals to educate patients about the importance of blood pressure control and the benefits of maintaining optimal levels. By actively engaging in regular monitoring, individuals can take charge of their health and reduce the risk of cardiovascular complications associated with hypertension.
Lifestyle Factors That Contribute to Hypertension
This paragraph will discuss two lifestyle factors that contribute to hypertension: diet and nutrition, and sedentary lifestyle and lack of exercise.
Diet and nutrition play a crucial role in the development and management of hypertension. Poor dietary choices, such as a high intake of sodium and low intake of fruits and vegetables, can increase blood pressure levels.
Additionally, a sedentary lifestyle and lack of exercise are also significant risk factors for hypertension, as physical activity helps to lower blood pressure and improve overall cardiovascular health.
Diet and nutrition
A well-balanced diet and proper nutrition play a crucial role in managing hypertension and reducing the risk of cardiovascular disease. Healthy eating habits, such as consuming fruits, vegetables, whole grains, and lean proteins, can help control blood pressure levels. Additionally, limiting salt intake is essential as excessive sodium consumption can increase blood pressure. A low-sodium diet can be achieved by avoiding processed foods, canned soups, and fast food, which tend to be high in sodium. To further support cardiovascular health, individuals should also focus on consuming foods rich in potassium, magnesium, and calcium, as these minerals have been linked to lower blood pressure levels. Overall, adopting a healthy diet and making mindful food choices can significantly contribute to the prevention and management of hypertension, ultimately reducing the risk of cardiovascular disease.
| Food Group | Recommended Servings | Examples |
|---|---|---|
| Fruits | 2-4 servings per day | Apples, oranges, bananas |
| Vegetables | 3-5 servings per day | Spinach, broccoli, carrots |
| Whole Grains | 6-8 servings per day | Brown rice, whole wheat bread, oats |
| Lean Proteins | 2-3 servings per day | Chicken breast, fish, tofu |
| Low-fat Dairy | 2-3 servings per day | Milk, yogurt, cheese |
Sedentary lifestyle and lack of exercise
Sedentary lifestyles and lack of exercise can have detrimental effects on overall health and well-being, leaving individuals vulnerable to various preventable health conditions. Research has consistently shown that a sedentary lifestyle increases the risk of developing hypertension, a major risk factor for cardiovascular disease.
Physical inactivity leads to weight gain, which in turn puts additional strain on the cardiovascular system. Moreover, lack of exercise weakens the heart and reduces its ability to pump blood efficiently, leading to increased blood pressure. Additionally, a sedentary lifestyle is often associated with poor dietary habits, further exacerbating the risk of hypertension.
Engaging in regular physical activity, on the other hand, promotes cardiovascular health by improving blood flow, reducing blood pressure, and maintaining a healthy weight. Therefore, incorporating regular exercise into daily routines is crucial for preventing hypertension and reducing the risk of cardiovascular disease.
Prevention Strategies for Hypertension and Cardiovascular Disease
Implementing effective prevention strategies is crucial in reducing the risk of both hypertension and cardiovascular disease. Lifestyle modifications play a significant role in preventing and managing these conditions.
Engaging in regular physical activity is essential, as it helps maintain a healthy weight, lowers blood pressure, and improves cardiovascular health. Incorporating aerobic exercises, such as walking, swimming, or cycling, for at least 150 minutes per week is recommended.
Additionally, adopting a healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, which emphasizes fruits, vegetables, whole grains, lean proteins, and low-fat dairy products, can help lower blood pressure and reduce the risk of cardiovascular disease.
Limiting alcohol consumption, quitting smoking, and managing stress through techniques like mindfulness and relaxation exercises are also important lifestyle modifications to prevent hypertension and cardiovascular disease.
By implementing these prevention strategies, individuals can significantly reduce their risk and improve their overall cardiovascular health.
Frequently Asked Questions
What are the symptoms of hypertension?
The symptoms of hypertension include high blood pressure, headaches, dizziness, chest pain, and shortness of breath. Causes of hypertension vary and may include lifestyle factors, genetics, and certain medical conditions. Treatment options include medication, lifestyle changes, and managing underlying health conditions.
How does hypertension affect the kidneys?
Hypertension can lead to kidney damage and impaired renal function. The elevated blood pressure puts strain on the blood vessels in the kidneys, reducing their ability to effectively filter waste products and maintain fluid balance.
Can hypertension be cured?
Hypertension can be managed but not completely cured. Treatment typically involves lifestyle changes such as maintaining a healthy weight, reducing sodium intake, exercising regularly, and managing stress. Medications may also be prescribed to control blood pressure.
What are the long-term effects of hypertension on the brain?
Long-term consequences of hypertension on the brain include cognitive decline. Hypertension can lead to damage to blood vessels in the brain, impairing blood flow and causing cognitive impairments such as memory loss and decreased cognitive function.
Are there any natural remedies or alternative treatments for hypertension?
Natural remedies and alternative treatments for hypertension include lifestyle modifications such as regular exercise, adopting a healthy diet, reducing stress, and avoiding tobacco and excessive alcohol consumption. Some herbal supplements like garlic extract and hawthorn may also have mild blood pressure-lowering effects.