Why Hypertension Is Linked To Rheumatic Heart Disease?
Hypertension, commonly known as high blood pressure, is a prevalent cardiovascular condition that affects a significant portion of the global population. Its association with various heart diseases has been extensively studied, including its link to rheumatic heart disease (RHD).
Rheumatic heart disease is a chronic inflammatory condition of the heart valves, primarily caused by rheumatic fever, an autoimmune response to a prior streptococcal infection.
This article aims to explore the relationship between hypertension and RHD, shedding light on the shared risk factors and the role of inflammation in the development of RHD. Furthermore, it will discuss the importance of early detection and intervention, as well as preventive measures to protect heart health.
Collaborating with healthcare professionals for comprehensive care is crucial in managing hypertension and preventing the onset or progression of RHD. Understanding the connection between hypertension and RHD is imperative in developing effective strategies for prevention, diagnosis, and treatment of these conditions.
Key Takeaways
- Hypertension is linked to rheumatic heart disease due to complications.
- Smoking raises blood pressure and damages blood vessels, increasing the risk of heart disease.
- Healthy lifestyle modifications, such as a balanced diet and regular exercise, can lower the risk of developing heart disease.
- Collaboration with healthcare professionals, including doctors, nurses, and healthcare providers, is crucial in developing personalized treatment plans and supporting patients in managing their conditions.
Understanding Hypertension and Its Effects on the Heart
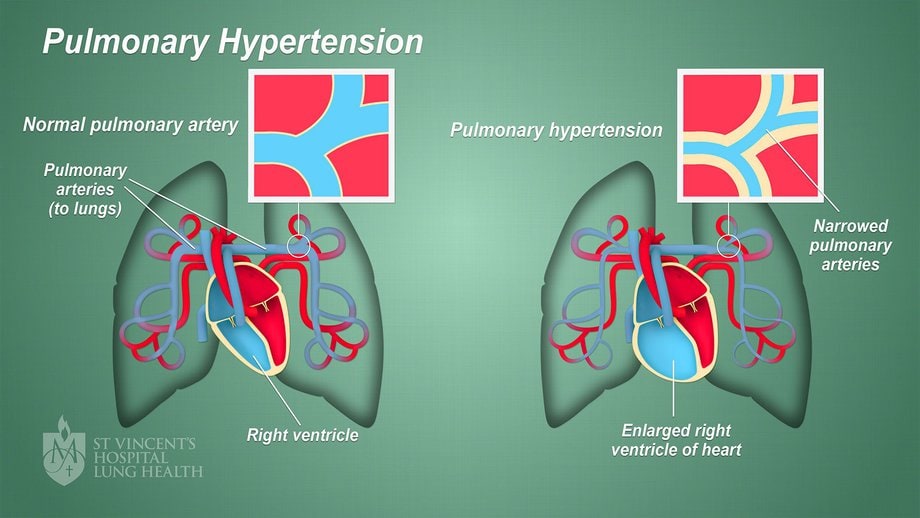
Hypertension, a condition characterized by high blood pressure, has been extensively studied due to its detrimental effects on the cardiovascular system, particularly on the heart.
The long-term complications of hypertension are well-documented and pose a significant risk to heart health. One of the primary effects of medication used to treat hypertension is the reduction of blood pressure levels, which helps alleviate the strain on the heart. By lowering blood pressure, these medications reduce the workload on the heart, decreasing the risk of complications such as hypertensive heart disease, heart failure, and coronary artery disease.
However, if left untreated or poorly managed, hypertension can lead to serious complications, including rheumatic heart disease. Therefore, understanding the effects of hypertension on the heart is crucial in preventing the development of associated diseases and ensuring optimal cardiovascular health.
Exploring the Relationship Between Hypertension and Rheumatic Heart Disease
Research has uncovered a significant correlation between elevated blood pressure and the development of cardiac complications associated with a particular inflammatory condition affecting the cardiovascular system. This condition, known as rheumatic heart disease (RHD), is a consequence of untreated or inadequately treated streptococcal throat infections. Hypertension, or high blood pressure, puts additional strain on the heart, leading to increased risks of RHD. The relationship between hypertension and RHD is complex, with hypertension contributing to the progression and severity of RHD.
Exploring prevention strategies for hypertension is crucial in reducing the risk of developing RHD. Lifestyle modifications, such as maintaining a healthy diet, regular exercise, and avoiding smoking and excessive alcohol consumption, can help in controlling blood pressure levels. Early detection and treatment of hypertension are also important to prevent further complications.
The long-term effects of hypertension on RHD are substantial. Uncontrolled hypertension can lead to progressive damage to the heart valves, increasing the risk of valve regurgitation or stenosis. This can result in heart failure, arrhythmias, and even death if left untreated. Therefore, it is essential to manage hypertension effectively to mitigate the development and progression of RHD.
| Prevention Strategies | Long-Term Effects |
|---|---|
| Healthy diet | Heart failure |
| Regular exercise | Arrhythmias |
| Avoid smoking | Valve abnormalities |
| Moderate alcohol consumption | Increased mortality |
Shared risk factors between elevated blood pressure and the development of cardiac complications associated with a particular inflammatory condition affecting the cardiovascular system have been identified. These shared risk factors highlight the importance of understanding the relationship between hypertension and rheumatic heart disease in order to implement effective preventive measures.
- Sedentary lifestyle: Lack of physical activity increases the risk of both hypertension and rheumatic heart disease.
- Unhealthy diet: Consuming a diet high in sodium, saturated fats, and processed foods is linked to the development of both conditions.
- Obesity: Excess body weight puts strain on the heart and increases the risk of developing hypertension and rheumatic heart disease.
- Smoking: Tobacco use damages the blood vessels and increases the likelihood of developing both conditions.
By addressing these shared risk factors, individuals can reduce their risk of developing hypertension and rheumatic heart disease. Implementing preventive measures such as regular exercise, adopting a healthy diet, maintaining a healthy weight, and quitting smoking can significantly decrease the incidence of these conditions.
The Role of Inflammation in Rheumatic Heart Disease
Inflammation plays a crucial role in the pathogenesis of rheumatic heart disease (RHD), a cardiovascular condition that can have devastating consequences on the health and well-being of individuals.
The immune response triggered by group A Streptococcus infection is a key factor in the development of RHD. When the body reacts to the infection, the immune system produces antibodies that not only target the bacteria but also cross-react with proteins in the heart valves, leading to inflammation.
This chronic inflammation can result in scarring and thickening of the heart valves, impairing their function.
Additionally, genetic factors have been found to contribute to the susceptibility to RHD. Certain gene variants have been associated with an increased risk of developing the disease, highlighting the complex interplay between genetic predisposition and immune response in the pathogenesis of RHD.
Treating and Managing Hypertension to Prevent Rheumatic Heart Disease
The effective management of elevated blood pressure levels can significantly reduce the risk of developing complications associated with cardiovascular conditions such as rheumatic heart disease. Treating hypertension is a crucial aspect of preventing the progression of rheumatic heart disease.
Here are three lifestyle modifications that can help in managing hypertension:
- Adopting a healthy diet: Consuming a diet rich in fruits, vegetables, whole grains, and low-fat dairy products can lower blood pressure levels. Limiting the intake of sodium, saturated fats, and cholesterol is also important.
- Regular physical activity: Engaging in regular exercise, such as brisk walking, swimming, or cycling, can help lower blood pressure. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week.
- Weight management: Maintaining a healthy weight through a combination of a balanced diet and regular exercise can significantly reduce blood pressure.
By implementing these lifestyle modifications, individuals can effectively manage hypertension and reduce the risk of developing complications associated with rheumatic heart disease.
The Importance of Early Detection and Intervention
Early detection and intervention play a critical role in preventing and mitigating the devastating consequences of cardiovascular complications. When it comes to hypertension and its link to rheumatic heart disease (RHD), early detection and intervention become even more crucial.
Screening for hypertension allows healthcare providers to identify individuals who are at risk of developing RHD. This allows for timely intervention and treatment to prevent the progression of RHD. Additionally, early intervention in hypertensive patients can help manage blood pressure levels, reducing the strain on the heart and minimizing the risk of developing RHD.
Regular screenings and early intervention strategies, such as lifestyle modifications and medication, can effectively control hypertension and prevent the onset of RHD. Therefore, the importance of screening and early intervention cannot be overstated in reducing the burden of RHD among hypertensive individuals.
Preventive Measures to Protect Heart Health
This paragraph introduces a discussion on preventive measures to protect heart health, specifically focusing on healthy diet and exercise, managing stress, and avoiding smoking.
These measures are important in maintaining a healthy heart and reducing the risk of developing heart-related diseases.
By following a balanced diet, engaging in regular physical activity, and adopting stress management techniques, individuals can promote their cardiovascular well-being and decrease the likelihood of heart-related complications.
Additionally, avoiding smoking is crucial as it is a major risk factor for heart disease and can cause significant damage to the cardiovascular system.
Healthy Diet and Exercise
Regular physical activity and a balanced diet that includes nutrient-rich foods are essential for maintaining cardiovascular health and reducing the risk of developing rheumatic heart disease in individuals with hypertension. Engaging in regular exercise helps to improve blood circulation, strengthen the heart muscle, and lower blood pressure levels.
A healthy diet, consisting of fruits, vegetables, whole grains, lean proteins, and low-fat dairy products, provides essential nutrients and helps to maintain a healthy weight.
Here are three important lifestyle modifications that can help individuals with hypertension to protect their heart health:
- Decrease sodium intake: Reducing the consumption of sodium-rich foods helps to lower blood pressure levels.
- Limit saturated and trans fats: Consuming foods high in saturated and trans fats can increase the risk of heart disease. Opting for healthier fats, such as unsaturated fats found in olive oil and avocados, is recommended.
- Increase physical activity: Engaging in moderate-intensity aerobic activities for at least 150 minutes per week can significantly improve cardiovascular health and reduce the risk of developing heart disease.
Managing Stress and Avoiding Smoking
One important aspect of maintaining cardiovascular health and reducing the risk of developing complications is effectively managing stress levels and abstaining from smoking.
Managing stress is crucial in preventing the progression of hypertension and subsequent development of rheumatic heart disease. Chronic stress can lead to an increase in blood pressure, which places additional strain on the heart and blood vessels. This can cause damage to the heart valves, leading to rheumatic heart disease.
Therefore, adopting stress management techniques such as exercise, meditation, and relaxation techniques can help in reducing blood pressure and minimizing the risk of complications.
Additionally, quitting smoking is also essential as smoking not only raises blood pressure but also damages the blood vessels, increasing the likelihood of developing heart disease.
By managing stress and quitting smoking, individuals can significantly decrease their risk of developing hypertension and its associated complications, including rheumatic heart disease.
Collaborating with Healthcare Professionals for Comprehensive Care
Collaborating with healthcare professionals is crucial for providing comprehensive care for patients with hypertension and rheumatic heart disease. A collaborative approach involving doctors, nurses, and other healthcare providers ensures that patients receive the best possible care and management for their conditions. This approach allows for a multidisciplinary team to work together, combining their expertise and knowledge to develop personalized treatment plans and strategies.
To emphasize the importance of collaboration and patient education, the following three points should be considered:
- Shared Decision Making: Collaborating with patients in decision-making processes empowers them and promotes a sense of ownership over their health. Patients should be actively involved in setting treatment goals and making informed choices regarding their care.
- Education and Support: Healthcare professionals should provide patients with resources and information about hypertension and rheumatic heart disease. This includes explaining the conditions, their causes, symptoms, and potential complications. Additionally, patients should be educated on lifestyle modifications, medication adherence, and regular follow-up care.
- Regular Communication: Effective communication between healthcare professionals and patients is crucial. Regular check-ins, follow-up appointments, and open lines of communication ensure that patients are supported in managing their conditions and any potential complications.
By adopting a collaborative approach and focusing on patient education, healthcare professionals can provide comprehensive care that improves outcomes and enhances the overall well-being of patients with hypertension and rheumatic heart disease.
Frequently Asked Questions
What are the symptoms of hypertension and how does it affect the heart?
Hypertension symptoms may include headaches, shortness of breath, and chest pain. It affects the heart by causing increased workload, leading to thickening of the heart muscles and narrowing of blood vessels, which can result in heart failure or heart attack.
Is there a cure for rheumatic heart disease?
There is currently no cure for rheumatic heart disease (RHD), but treatment options aim to manage symptoms, prevent further damage to the heart, and reduce the risk of complications. These may include medications, such as antibiotics to treat infections and anti-inflammatory drugs to reduce inflammation. In some cases, surgery may be necessary to repair or replace damaged heart valves.
Can rheumatic heart disease be prevented through lifestyle changes and medication?
Prevention methods for rheumatic heart disease include regular medical check-ups, adherence to antibiotic prophylaxis, and lifestyle changes such as a healthy diet and exercise. Medications, such as antibiotics and anti-inflammatory drugs, can effectively prevent and manage the disease.
How does inflammation contribute to the development of rheumatic heart disease?
Inflammatory response and immune system activation play a key role in the development of rheumatic heart disease. The inflammatory process triggered by the immune system’s response to an infection can lead to damage and scarring of the heart valves, resulting in the development of the disease.
What are the long-term complications of uncontrolled hypertension and rheumatic heart disease?
The long-term effects of uncontrolled hypertension and rheumatic heart disease include heart failure, stroke, and kidney damage. Management strategies for both conditions involve lifestyle modifications, medication adherence, and regular medical follow-up to prevent complications and improve overall health outcomes.